Diagnosis of Arteriovenous Malformation
Early and accurate diagnosis is crucial to understand the structure, location, and severity of an AVM and to plan the most effective treatment. The primary methods of diagnosis include:
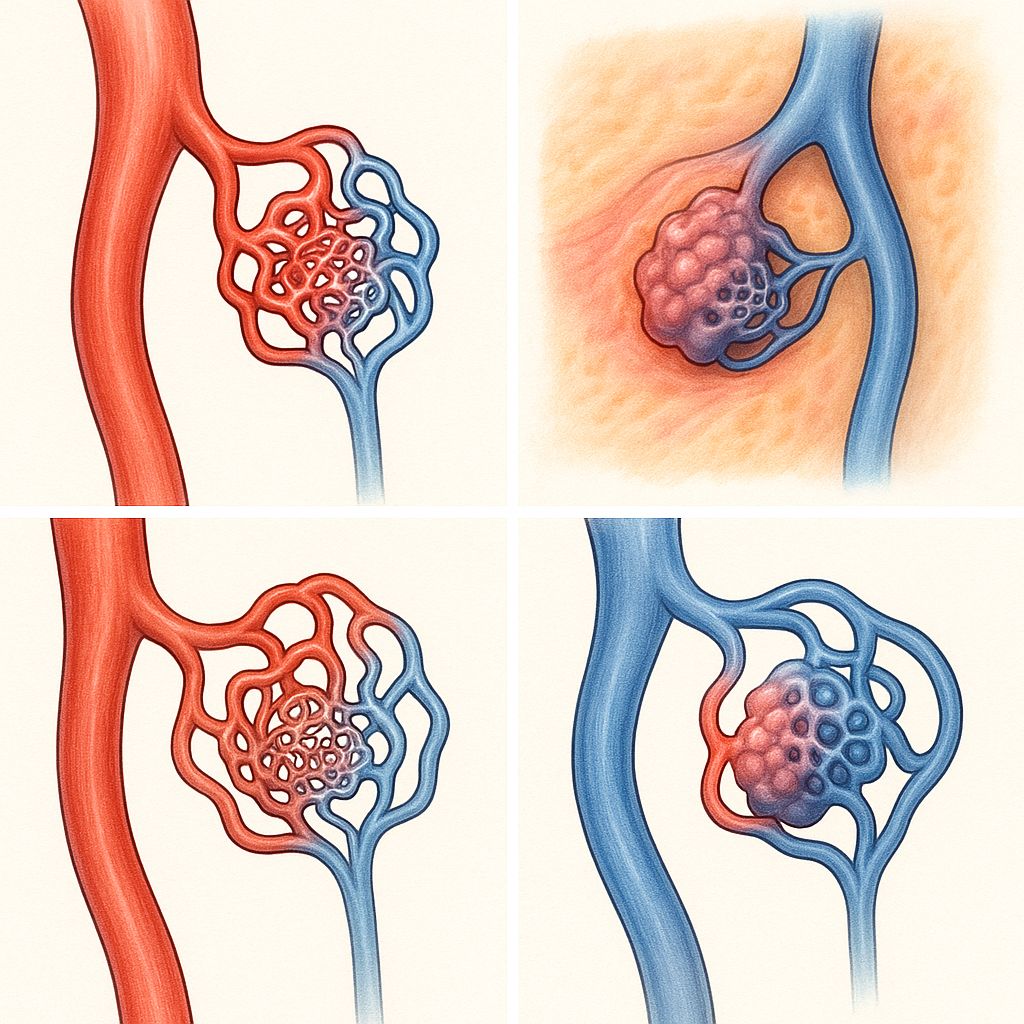
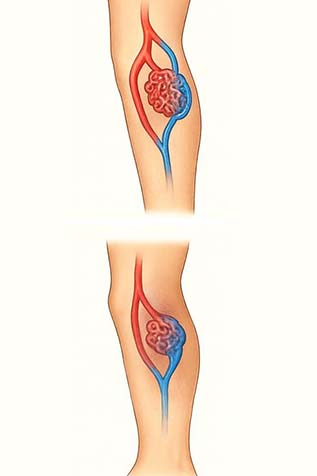
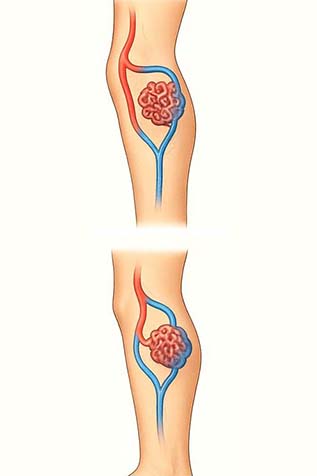
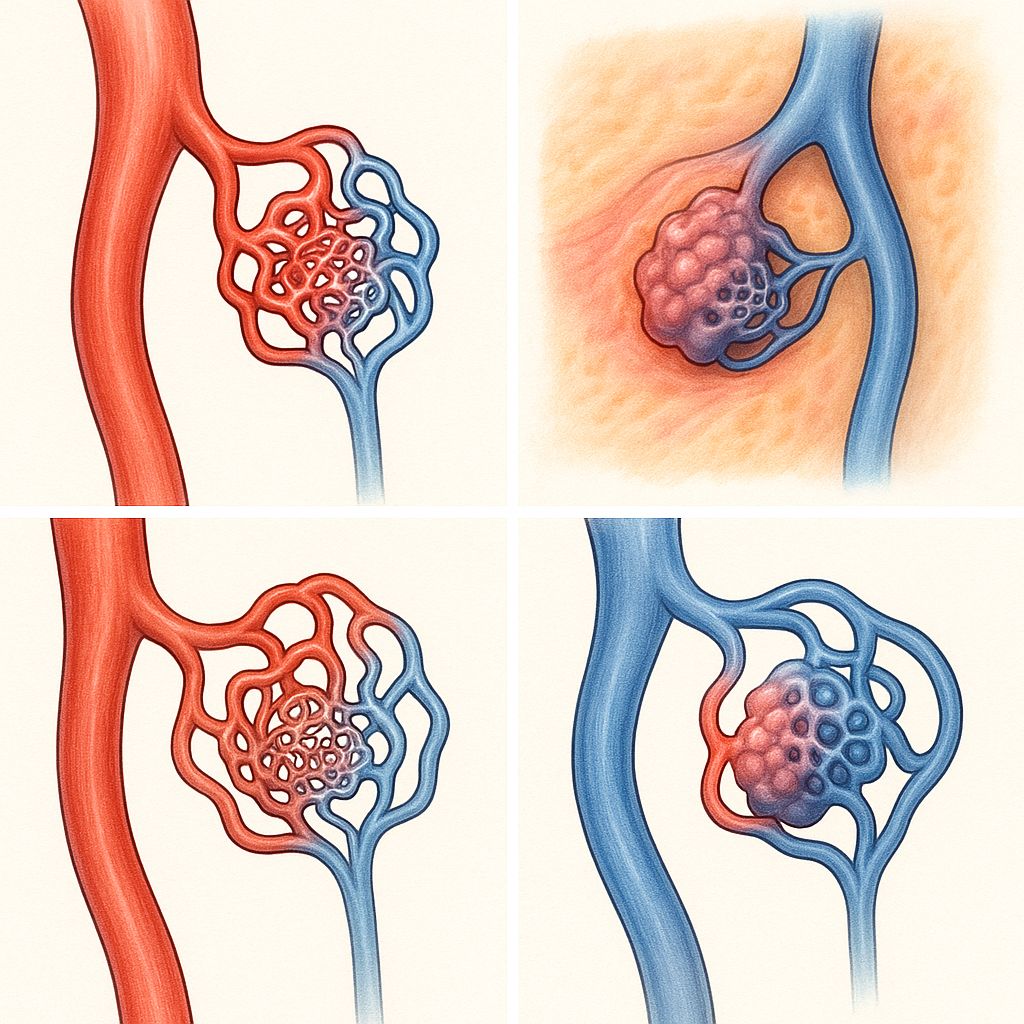
Arteriovenous Malformation (AVM) refers to an abnormal link between an artery and a vein within the limb’s vascular system. Normally, blood flows from arteries into smaller capillaries before reaching the veins, but in an AVM, this direct connection causes high-pressure arterial blood to rush into veins, making them swollen and twisted over time, similar in appearance to varicose veins, but much more complex in nature.
Unlike typical varicose veins caused by weak vein valves, AVMs are congenital (present from birth) and can worsen over time as the vessels expand under pressure. They may cause visible bulging veins, pain, warmth, skin discoloration, or even ulcers in the affected leg.
If untreated, an AVM can strain the heart or cause severe bleeding. Diagnosis is made using Doppler ultrasound or angiography, and treatment often involves embolization or surgical removal to block the abnormal vessels and restore normal venous circulation.

Most AVMs are present from birth, caused by improper blood vessel formation during fetal development.
Certain inherited conditions affecting blood vessel growth can increase the risk of AVMs.
Periods of hormonal fluctuation such as pregnancy or puberty can worsen vascular malformations and varicose veins.
Previous injuries or surgeries to blood vessels may trigger abnormal artery- vein connections.
Occupations or lifestyles involving long periods of standing can increase vein pressure and reveal underlying malformations.
Pre-existing vein problems like chronic venous insufficiency or varicose veins may aggravate or coexist with an AVM.
The classic type — a direct connection between arteries and veins without a capillary bed. It creates a high-flow system, often leading to bulging veins, pain, or bleeding.
A low-flow vascular malformation made up of abnormally dilated veins. These are often soft, compressible, and may cause swelling or pain, especially when standing or during activity.
Also known as “port-wine stains”, these are superficial abnormalities of small capillaries in the skin, causing flat, reddish discolorations. They may be purely cosmetic or associated with deeper vessel malformations.
A malformation of lymph vessels, leading to fluid-filled cysts or swelling. Though not directly linked to blood flow, they often coexist with venous or arteriovenous malformations in complex vascular cases.
Early and accurate diagnosis is crucial to understand the structure, location, and severity of an AVM and to plan the most effective treatment. The primary methods of diagnosis include:
A non-invasive test that uses sound waves to visualize blood flow within vessels. It helps detect abnormal connections between arteries and veins, assess flow patterns, and identify high- pressure zones typical of AVMs.
A detailed imaging technique where contrast dye is injected into the bloodstream to clearly map out the blood vessels. It allows doctors to pinpoint the size, depth, and feeding arteries or draining veins.
Treatment for AVM focuses on stopping abnormal blood flow, relieving symptoms, and preventing complications like bleeding or ulceration. The choice of treatment depends on the AVM’s size, location, and severity.
A minimally invasive procedure where a catheter is guided into the abnormal vessels, and special materials (such as glue, coils, or foam) are injected to block the abnormal blood flow and reduce pressure within the veins.
In cases where the AVM is well-defined and accessible, surgeons may remove the entire malformation to prevent recurrence or rupture.
A chemical injection therapy used to shrink or seal off the abnormal vessels by damaging their inner lining. It is commonly used for smaller or superficial AVMs, especially in the limbs.
A non-surgical, targeted radiation therapy that focuses high-dose beams on the AVM to gradually close off abnormal vessels over time..
Arteriovenous Malformation (AVM) is a complex vascular condition that demands timely diagnosis and expert management. Although most cases are congenital, recognizing its symptoms early—such as visible veins, swelling, or unexplained pain—can prevent serious complications like bleeding, ulceration, or heart strain. With advances in modern vascular care, treatments such as embolization, sclerotherapy, and minimally invasive surgery have made it possible to control and correct AVMs effectively. Adopting a healthy lifestyle, staying active, and attending regular vascular check-ups play a vital role in long-term management. Early medical attention and a personalized treatment plan not only reduce the risk of complications but also ensure better circulation, comfort, and overall vascular health for individuals living with AVM.
Got a question?

An AVM is an abnormal connection between arteries and veins that disrupts normal blood flow and oxygen circulation
Most AVMs are congenital, meaning they form before birth due to abnormal blood vessel development.
Symptoms may include headaches, seizures, muscle weakness, or bleeding in the affected area.
AVMs are diagnosed using imaging tests such as MRI, CT scan, or cerebral angiography.
Treatment options include surgery, endovascular embolization, or focused radiation therapy depending on its size and location.